Optometrists in Alberta seeking to expand scope of practice
/The Alberta College of Optometry (ACO) has submitted to Alberta Health & Wellness (AHW) a Proposal to amend the Optometrists Profession Regulation Respecting the Authorization to Perform Restricted Activities to include such things as manage patients with glaucoma without any involvement of Ophthalmologists including prescribing medications and performing laser iridotomies and trabeculoplasties. I would be interested in feedback regarding this issue from both Optometrists and Ophthalmologists who care for glaucoma patients and how this effects inter-professional collaboration for the best care of our patients.
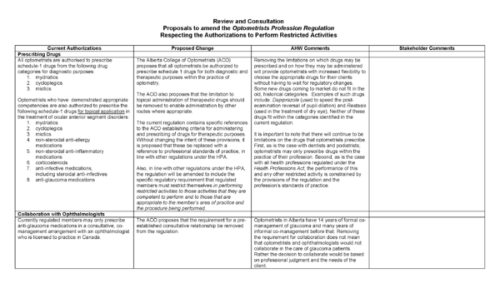
Clicking on the thumbnail downloads the three page PDF file of the proposed changes in the Optometry regulation act for glaucoma care.
The subject of what optometrists do, their own desire to be independent and collaborating with other eye care professionals (ECPs) are complex issues that impact this movement of scope of care expansion through legislative means.
I think that organized ophthalmology's longstanding bias and lack of acceptance of optometry has been borne out of a blend of patient concern, financiall insecurity, and a pereception of optometric education. All of these bear upon optometry in veracity far outweighing the realities, though. While there are untrained individuals who can do a variety of "medical" and "surgical" procedures (such as skin and eyelid tattoos), the resistance to optometric expansion of care is inconceivable to many optometrists.
In the current circumstance, an overall brilliant track record of optometric medical eye care in the US, the level of education in both US and Canadian optometry schools and disparity of geographic availability of eye care should not alarm ophthalmologists anywhere. Frankly, in my city where median household incomes are six times the poverty level, medical eye care for 80,000 underinsured or uninsured has a waiting period of almost 1 year. And this area has one of the highest densities of ophthalmologists in CA (with Stanford Medical School and UC San Francisco Medical School as bookends). In rural Canada and the US it's probably equivalent.
I think from the record, there is no reckoning that optometry has not done a yeoman's job of providing basic and even intermediate medical eye care. The galling aspect of this experience has been organized ophthalmology's discounting of this experience. There are admittedly exceptions to the rule, but these are exceptions that would also normally occur in any profession where professional judgement or negligence is probable.
I think that this request for expansion of care by Alberta optometrists should not be feared by ophthalmologists for the following reasons:
- Most optometrists are not interested or compelled to perform any(!) kind of surgical procedure. Therefore, ther request is likely an attention getter and a negotiating step. It was proffered on the basis of past experiences of the response from ophthalmology for any(!) scope expansion.
- Most optometrists do not have the capital to fund the complex equipment and infrastructure to exploit the full benefits of any kind of surgical procedure.
- Most optometrists are generally risk averse by nature and are completely bound by their training and experience.
- Most optometrists who would employ expanded scope of care would provide a tremendous social benefit to their jurisdictions and would have absolutely no financial impact on the the ophthalmologists.
In summary, I think that Canada has an opportunity that is unexcelled in the US. There is an excellent opportunity for both ophthalmology and optometry to collaborate and by working with each other. Rather than splintering further, by toning down the inflammatory rhetoric and working together, I think that ophthalmology would even see greater revenue by reinforcing the collaborative relationships that now exist.
Update on Friday, July 22, 2011 at 1:06PM by Robert M Schertzer, MD, MEd, FRCSC
(The following comments were copied from original submission dates and posted as a journal follow-up article in preparation for changing to DISQUS for future commenting on my blog.)
18Jan2010 reader comment:
Rob,
I have practiced in states (Virginia) that required collaboration before treating glaucoma and states (North Carolina, New Mexico) that do not. It was most inconvenient for me, the ophthalmologist, and especially the patient when I had to ask permission to start someone on a therapy. Luckily VA changed their laws allowing optometrists to practice to the full extent of our training. In no way did this end collaboration. I would still refer out patients who had progressive field loss or non-responsive to therapy or non-compliant, etc.
Personally, I don't have the need or desire to perform SLT or PIs. However, I have plenty of close MDs nearby who take these referrals and return the patients to my care. If I were in a more rural area, I would get the additional training (of course, that is dependent on the state).
ODs and MDs can and do thrive when they work together.
Jeff Sterling, OD
jeffrey.sterling@doctorsvisioncenter.com
18Jan2010 my response:
Thanks for posting your concern Kam. Please note that the title of the document in the paragraph above the thumbnails is actually a link to download a PDF version of the document (if you hover your mouse over it, you should see a pop-up telling you that this will do just that.) The images were just meant as thumbnails and I posted them as wide as possible so that they would still fill the width of my blog but, as you pointed out, this is still not very readable.
To make this easier, I have now changed it so that clicking on any of the three thumbnails will all bring up the same 3-page PDF document. I hope this makes it easier for others to understand.
Robert M Schertzer, MD, MEd, FRCSC
18Jan2010 I added:
Thanks so much Jeff for posting your first-hand experience in two different practice situations in collaborating with ophthalmologists in caring for glaucoma patients. I believe you hit upon a key point and that is that there is much in the way of regional differences in the delivery of quality eye care to our patients depending on the availability of different types eye care professionals.
For example, in the maritime region of Canada (on the east coast), there is a relative shortage of ophthalmologists making it essential for optometrists to provide much of the primary eye care. Our bigger cities tend to have more Ophthalmologists and, as one would expect, most of the sub-specialist ophthalmologists. Unlike the States, I am not aware of any sub-specialized Optometrists, at least not in the Vancouver, BC area where I practice.
As you know, there can be some 'competition' between optometrists and general ophthalmologists for primary eye care. Glaucoma accounts for 1/3 visits to general ophthalmologists yet optometrists tend to, when seeking an ophthalmologist's opinion on the care of a glaucoma patient, refer exclusively to a glaucoma sub-specialized ophthalmologist rather than to a general ophthalmologist.
The bottom line is that it is really quite a complex issue with so many regional variations in the delivery of eye care to glaucoma patients and potential side effects to treatments. Yes indeed, there are overlapping roles, and I hope when all is settled, glaucoma patients are getting the best care possible. If any eye care provider is properly qualified that is good, especially when they know when to refer knowing that we all are working together for the good of our patients. There are systemic implications of all medications, even topical ones, that need to be fully understood. Also, those not performing glaucoma surgery may not realize when it might be beneficial to opt for surgery early; of course even a general ophthalmologist or one in another sub-specialty area can miss this as well. Ophthalmologists have had 9-11 years of training beyond Optometrists (medical school, internship, residency, then optional fellowship) all dealing with systemic diseases, medical and surgical therapy. It is still important that this background can be called upon to help when patients need our help.
Robert M Schertzer, MD, MEd, FRCSC
19Jan2010 reader comment:
Hi Rob
I would like to say thanks for having a discussion about this topic with so many sides and angles. A few comments; we need to keep the facts as accurate as possible to have the best chance at a reasoned discussion. Typical ODs and OMDs both have undergraduate degrees and then 4 year professional school programs. OMDs typically have 5 years of additional training, the length of the residency programs here in Canada. Some OMDs go on to do fellowships, typically 2 year programs. About 10% of North American trained optometrists do an optional 1 year residency training program, and a few do 1 or 2 year fellowships. So, on average, the difference in education in years is likely 5-7. The total amount of time spent during medical school in ophthalmology was one week or less for 76.2% of resident respondents as reported here Can J Ophthalmol. 2009 Oct;44(5):513-8.
Peter J McDonnell, the director of Wilmer's Eye, wrote an interesting Op-ed that can be viewed here http://www.modernmedicine.com/modernmedicine/article/articleDetail.jsp?ts=1263964262659&id=398681. In summary, he says that too much time and money is spent teaching future OMDs things that will have no impact on their careers (as he reports they didn't on his). His solution is to shorten training times and restrict the information taught to that germane to eyecare. (almost sounds like optometry school with a surgical residency)
It is interesting to note that there is at least one dental school (Arthur A. Dugoni School of Dentistry) in San Francisco that has a 5 year program that students can enter straight out of high school. These kids graduate before ODs and OMDs alike, as surgeons, administering anaesthesia and prescribing any drugs that are needed for oral health care, including many that have serious systemic side effects. They do this despite not having spent one day in medical school.
There are alternative means to an end. Contemporary optometry school is one of the ways, a much shorter way, to train competent eye doctors in many areas of ocular health, including independent glaucoma care. The quality of the care received by the patient is often more dependent on clinical/ethical judgements than the degree received. Those that keep the patient's best interest at the center of their decision making will almost always be a good doctor. They will treat what they are competent to treat, and they will refer when they are outside of their comfort zone/competency. Just as most OMDs choose not to do retinal surgery, many ODs will choose not to treat glaucoma. I hope that all practitioners, regardless of their degree or scope of practice, know there own limitations and stay within them. The proposed increase in scope of practice is an opportunity for those optometrists with the required competencies to broaden their spectrum of clinical care for the benefit of their patients. This increase in scope would be playing catch-up (after many years) to most of the United States when it comes to glaucoma management. The laser and minor surgical procedures are authorised in several states through legislation, but they are practised in many more states within the federal health system.
I have been a part of great OD/OMD teams in Arizona that are the way of the future given the manpower concerns, the aging population, and the quality of the optometric education. The legislation change would bring us one step closer.
Lastly, there is an unfortunate reference to PDT for hemangioma in the proposal to expand scope of practice that you have linked. That was not contemplated nor intended to be in the document. It was an error. It should be stricken from the document and the discussion.
Mark Bourdeau BSc, OD, FAAO
19Jan2010 my response:
Thanks so much Mark for the clarification re number of years and other points. My understanding here in Canada at the only two optometric programs is that Optometry is an undergraduate degree...hence the 9-11 year figure I came up with vs the 5-7 years. That being said, we all have so much to offer our patients.
Robert M Schertzer, MD, MEd, FRCSC
2Jun2010 a 'concerned ophthalmologist' wrote:
I have concerns with the proposed expanding scope of optometrists. An ophthalmologists training consists initially of years in medical school where one is trained to diagnose and manage people with acute illnesses. During medical school, one sees both the benefits and the occasional severe side effects of the medications we use. Almost every patient we deal with is sick enough that they are hospitalized. We learn to rely on our own judgement and are not simply observers.
In an ophthalmology residency, again the acuteness of illness exists. That is, we are seeing and managing patients with real ocular disease 99.9% of the time. Granted, when finished training, the acuteness of ocular disease is often greatly reduced in a regular day in a general ophthalmology practice.
I challenge that in optometry school, these ratios are reversed. One is often seeing screening ocular exams, refractions, etc, and the amount of real vision threatening and life threatening disease is seen on rare occasions. Granted, many optometrists often obtain experience in hospitals or working with ophthalmologists, but this is often in an observership capacity. I feel that just to watch others and read about things in books, can never replace the years of experience and long hours of dealing with acute disease that an ophthalmologist experiences.
So that all being said, I do not agree with the expansion of scope of practice.
concerned ophthalmologist
2Jun2010 to which Dr Hom responded:
Dear anonymous and concerned ophthalmologist,
Thanks for posting a response. I can understand your view point but I must point out that the view or perception you have about optometric education may be dated. In addition, as an optometrist who has treated many, many medical eye problems, Therefore, modern optometric education can meet the guidelines of most of your concerns.
Secondly, I think a small portion of your concern might be related to the lack of follow through that you might think optometrists have. Or whether they would be callous or dismissive of the importance of this kind of responsibility. I beg also to differ that the new optometrist of the last 10 or even 15 years is a conscientious practitioner.
I would also submit that a collaborative co -management relationship can be financially and intellectually rewarding to any ophthalmologist,especially in the environment of premium IOLs and refractive surgery.
I ask only that you open your mind and consider a new view.
Kind Regards.
"...I challenge that in optometry school, these ratios are reversed. One is often seeing screening ocular exams, refractions, etc, and the amount of real vision threatening and life threatening disease is seen on rare occasions. Granted, many optometrists often obtain experience in hospitals or working with ophthalmologists, but this is often in an observership capacity..."
Richard Hom OD
richard@GrandRounds4ODs.com
http://GrandRounds4ODs.com
2Jun2010 my last word for now:
Great discussion starting to happen here and there are valid and important points by both Dr Hom and Anonymous Ophthalmologist. Yes, ophthalmologists do have more training in dealing with patients with chronic medical illnesses vs patients earlier in the course of disease at least here in Vancovuer. This however is not at all the same in many other parts of the world outside our tertiary care zone in our suburban setting.
Even using the argument that optoms see healthier patients vs sicker ones for EyeMDs, this may not mean that optoms should not prescribe glaucoma drops...if you would allow me to be devil's advocate for a moment. Dr Hom has actually made a similar argument before in some of his postings namely that if ophthalmologists see sicker patients, they need more time to do surgery and have less time for primary eye care. If optoms were helping manage patients with glaucoma earlier in the course of their disease, wouldn't this free ophthalmologists up to deal with the patients who need their surgical expertise?
There is room for working together between optometrists and ophthalmologists in caring for patients with glaucoma by making the patient the centre of attention, ie the Glaucoma Patient Centred model of eye care that is being developed in conjunction with the Canadian Glaucoma Society.
Robert M Schertzer, MD, MEd, FRCSC